Slipped/Herniated Disc
A slipped disc, also called a prolapsed or herniated disc, is when a soft cushion of tissue between the bones in your spine bulges outwards or when the disc moves from its natural position. It’s painful if it presses on spinal nerves.
Slipped discs affect roughly 1% to 3% of adults annually. It is most common in people aged 30 to 50 and men are affected twice as often as women.
Most cases resolve naturally within 6-12 weeks. However, 10% of patients with acute symptoms require surgical intervention.
Understanding Slipped & Herniated Discs
Symptoms
Slipped or herniated discs in the lumbar spine typically cause:
- Acute sciatica – persistent pain in the buttocks, hips or legs when the disc presses on the sciatic nerve
- Chronic band-like lumbar pain increased by exertion, driving, static sitting and standing, sometimes associated with bouts of complete spinal immobility
- Persistent lumbar back pain
- Significantly impaired mobility
- Problems bending or straightening your back
- Muscle weakness
Causes
- Degenerative disc disease – when the soft cushion of tissue (nucleus pulposus) in discs between the vertebrae in your spine pushes out, causing the disc to move from its natural position.
For more information, see our degenerative disc disease overview (PDF) - Ageing
- Exercising too hard
- Lifting heavy objects the wrong way
- Sitting down or driving for long periods of time
- Being inactive or overweight
Why Are You in Pain?
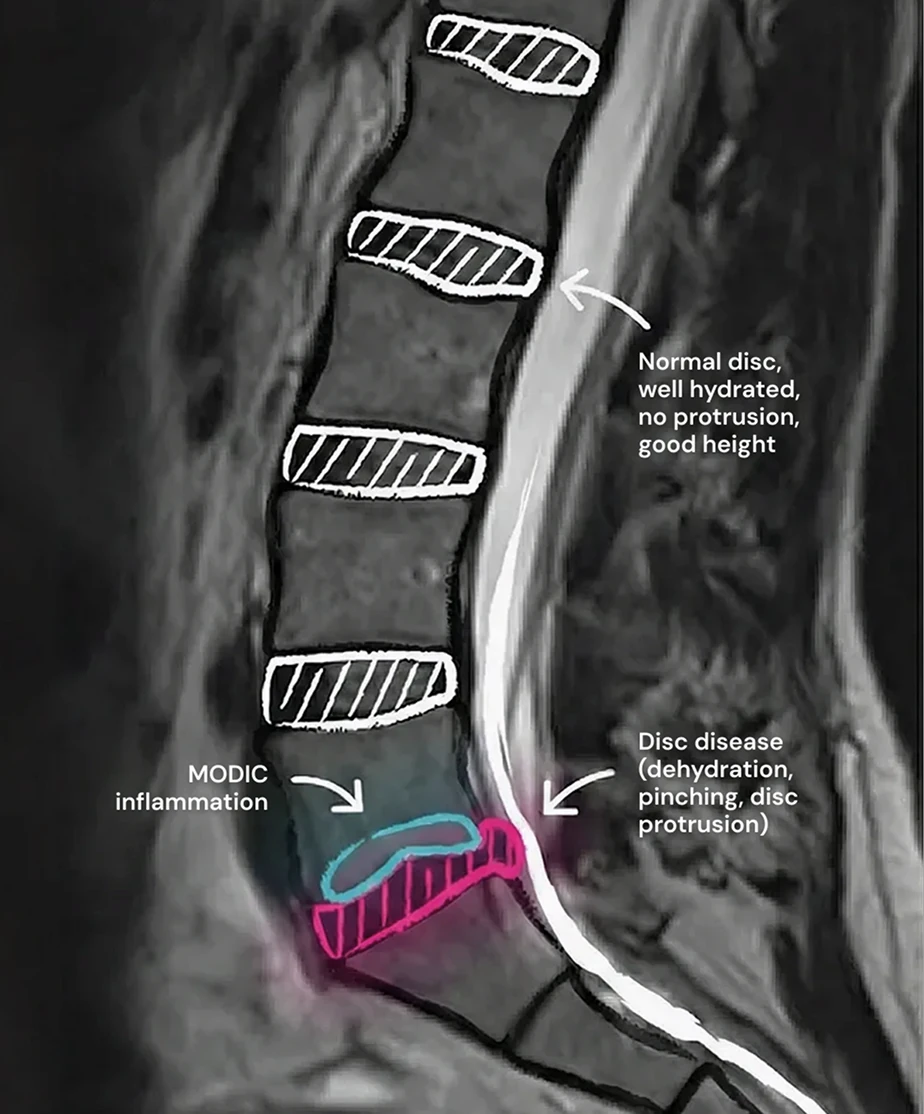
- Degeneration of a lumbar disc, due to multiple factors (genetic, postural, traumatic, overload, etc.)
- Degenerated disc fragments compressing nerves in the spinal cord resulting in chronic sciatica in one or both legs and gluteal region
- Disc pinching, with dehydrated, bulging (protrusion) and sometimes inflammatory
Do Slipped & Herniated Discs Heal on their Own?
Mild symptoms often resolve themselves. However, once repeat symptoms become acute, they normally continue to deteriorate until surgical intervention is required.

What Treatments are Available?
Treatments for slipped discs vary depending on the severity of the symptoms.
For mild cases, painkillers, physiotherapy and walking will help to resolve symptoms naturally.
If frequency and severity of symptoms increase, surgical intervention is often required.
Typical options available to patients are:
- Steroid injections to temporarily relieve symptoms by reducing inflammation around the slipped disc.
- Discectomy to relieve symptoms by removing disc fragments pressing on spinal nerves.
Discectomies often provide temporary symptom relief as further disc degeneration occurs allowing additional disc fragments to press on spinal nerves. - Spinal fusion which permanently fuses vertebrae together using titanium rods and screws allowing the degenerated disc to be removed.
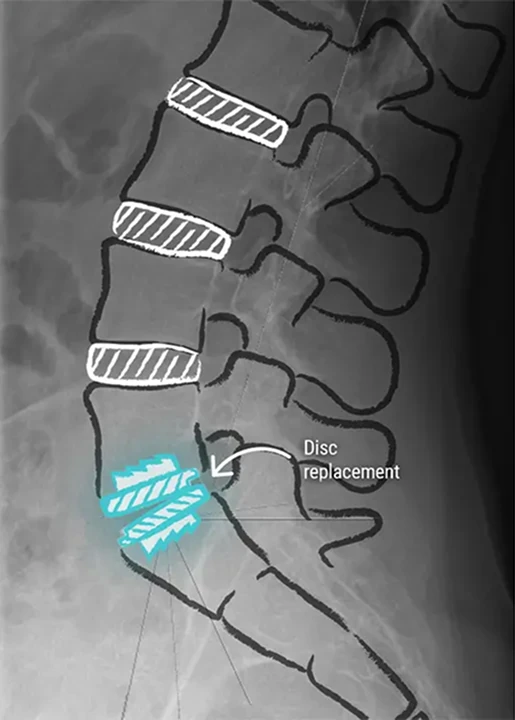
- Prodisc® L total lumbar disc replacement which replaces the degenerated natural disc with an artificial disc to restore spinal mobility and permanently relieve symptoms.
For further information on surgical options, please see our page on slipped & herniated disc treatment.